Pancreatitis after Gallbladder Removal: Incidence, Causes, and Mimics.
Our content is not intended nor recommended as a substitute for medical advice by your doctor. Use for informational purposes only.
Gallstones are one of the most common causes of pancreatitis.
Removing the gallbladder after an attack of gallstone pancreatitis is one of the most common scenarios in medicine.
If you are here because you are worried about the recurrence of pancreatitis after removing the gallbladder, then this article is for you.
What you need to know:
- Overall, the risk of pancreatitis decreases after gallbladder removal surgery.
- This is because of the removal of the gallstone-containing gallbladder during surgery. Small gallstones slipping from the gallbladder are the most common cause of pancreatitis.
- Recurrence of pancreatitis after cholecystectomy is rare, but it can occur.
- Common causes include missed or newly formed stones inside the common bile duct, alcoholism, medications, etc.
- Beware of conditions that mimic pancreatitis after gallbladder surgery, such as surgical wound complications, post-cholecystectomy syndrome, gastritis, etc.
- We diagnose pancreatitis after gallbladder symptoms based on characteristic pain, serum amylase & lipase, and abdominal imaging.
1. Can pancreatitis recur after gallbladder surgery?
Gallstones are the most common cause of acute pancreatitis. It accounts for 40 to 70% of pancreatitis (reference).
Removing your gallbladder after an attack of gallstone pancreatitis aims to decrease the recurrence of pancreatitis.
So, Gallbladder removal surgery protects you from future pancreatitis.
After a gallbladder operation, it is very rare to have pancreatitis. So, no need to worry about the condition.
It is extremely rare for gallstone pancreatitis to recur after gallbladder removal surgery. In such a case, the cause is often missed or newly developed stones after gallbladder removal.
For more details about gallstones after gallbladder removal, Read our in-depth article: Can you still get gallstones after gallbladder removal?
Also, you may get pancreatitis after gallbladder removal due to causes other than gallstones. Common causes include alcoholism, increased blood triglycerides, medications, and genetic factors.
The causes are discussed in the next sections.
2. What is the incidence of pancreatitis after gallbladder surgery?
Every year in the United States, up to 35 cases per 100,000 people get acute pancreatitis.
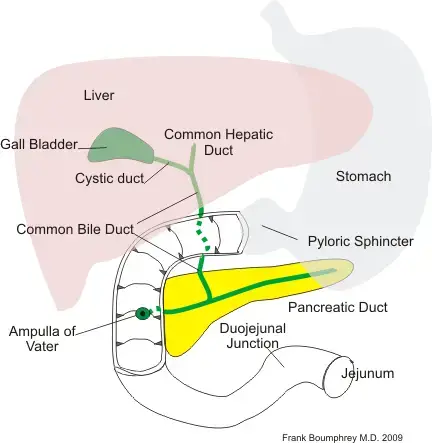
Most of these cases occur due to gallstones obstructing the pancreatic duct, causing pancreatitis.
Removal of the gallbladder is one of the preventive measures to reduce the risk of recurrence of acute pancreatitis.
So, pancreatitis rarely recurs after gallbladder surgery. The incidence of pancreatitis depends on its cause.
- Gallstone pancreatitis (pancreatitis due to gallstones obstructing the pancreas) incidence falls dramatically due to less risk of gallstones. However, it can occur if a new stone develops inside the bile ducts.
- The risk of pancreatitis due to other causes such as alcoholism and medications remains the same after cholecystectomy.
There is little data about the exact incidence of pancreatitis after gallbladder operations. However, in the early post-cholecystectomy period, only a few case reports of acute pancreatitis immediately after gallbladder removal.
One review study found that patients who undergo cholecystectomy after an attack of pancreatitis are at a much lower risk of pancreatitis recurrence. For example, the risk of pancreatitis recurrence dropped from 35.2% to 11.1% after cholecystectomy.
3. Common causes of pancreatitis after cholecystectomy?
Pancreatitis after gallbladder removal can be classified based on the time it occurs into:
- Early post-cholecystectomy pancreatitis (within days or a few weeks).
- Late post-cholecystectomy pancreatitis (occurring months or years after the gallbladder surgery.
Possible causes of early post-cholecystectomy pancreatitis include (reference):
- Slipped stone during the operation.
- The missed stone inside the common bile duct.
- Slipped bile sludge (sludge ball) into the CBD, reaching the pancreatic duct or the Ampulla of Vatter.
- Medications.
- Combined ERCP and cholecystectomy (post-ERCP pancreatitis).
Possible causes of late post-cholecystectomy pancreatitis:
- The newly developed stone is inside the biliary system (frequently inside the common bile duct).
- Alcoholism.
- Hypertriglyceridemia (increased blood triglycerides, especially in obese people).
- Some medications.
- Cancer in the head of the pancreas or the Ampulla of Vater.
- Increased blood calcium (hypercalcemia).
- Certain infections such as viruses (hepatitis B, Mumps, cytomegalovirus, etc.), Bacteria (mycoplasma, legionella, etc.), and parasites (Ascaris, toxoplasma, etc.).
- Unknown causes (acute idiopathic pancreatitis).
The overall risk of pancreatitis dramatically decreases after gallbladder surgery.
The reason behind this lower risk is the elimination of the major cause of gallstones by removing the gallbladder (remember, gallstones alone are responsible for up to 70% of the cases of acute pancreatitis).
4. Symptoms of pancreatitis after gallbladder removal?
In the first few days after a gallbladder removal operation, patients may suffer from post-operative pain due to the surgical wound or local complications such as infection.
If pancreatitis occurs during the early post-operative stage, it can be missed due to the similarities in symptoms.
So, it is important to know the typical symptoms of pancreatitis to help diagnose.
The typical symptoms of acute pancreatitis after gallbladder removal include:
- Pain location: Most patients have sudden onset of persistent severe upper central (epigastric) abdominal pain.
- Pain radiation: the pain often radiates to the left upper abdomen (left hypochondrium) and the center of the mid-back area. The pain may also radiate to the right upper abdomen in some patients.
- Relieving factors: the pain is often persistent for days, but it can be partially relieved by sitting up or leaning forward.
- Nausea and vomiting: in about 90% of the patients.
- Severe anorexia (loss of appetite).
- Tenderness and bloating in the upper abdomen.
- Fever.
- Difficulty breathing.
- Symptoms of complications such as low blood pressure, peeing too small (kidney failure), low oxygen (respiratory failure), coma, etc.
5. Common mimics of pancreatitis after gallbladder removal?
1. Post-cholecystectomy syndrome.
Post-cholecystectomy syndrome describes the persistence of abdominal pain and other symptoms that recur or persist after gallbladder surgery.
The pain can be severe, mimicking acute pancreatitis or gallbladder pain.
2. Post-operative complications of cholecystectomy.
Early complications after gallbladder removal may produce intense upper abdominal pain that mimics acute pancreatitis.
Examples of the complications:
- Surgical wound seroma or infection.
- Injury to the bile ducts or the site of attachment of the gallbladder to the liver (gallbladder bed).
- Bile duct injury or ligation.
- Post-operative hemorrhage.
- Bowel injury during the operation.
3. Gastritis and peptic ulcer disease.
Chronic gastritis and stomach and duodenum ulcers can cause extreme pain attacks mimicking acute pancreatitis.
4. Sphincter of Oddi dysfunction.
5. Irritable bowel syndrome.
6. Heart attack (inferior myocardial infarction).
Ischemia or infarction of the inferior part of the heart muscle can cause severe epigastric pain mimicking pancreatitis (reference).
7. Others:
Other conditions that mimic pancreatitis pain include acute cholangitis, GERD (acid reflux), gastroenteritis, IBS, IBD, etc.
6. Diagnosis of post-cholecystectomy pancreatitis.
As we explained, several conditions can mimic pancreatitis pain after gallbladder removal. Therefore, when your doctor suspects pancreatitis, he will order some investigation to confirm or exclude the condition.
Common investigations to diagnose pancreatitis include:
- Serum amylase and lipase.
- Abdominal sonography.
- Abdominal CT (Contrast-enhanced).
- Abdominal MRI.
- Liver enzymes (ALT, AST, Alkaline phosphatase).
- Bilirubin levels (total and direct).
- Full blood count.
- Others include trypsinogen activation peptide (TAP), urinary and serum trypsinogen test-2, etc.
The diagnosis of pancreatitis is established when you have 2 of the following three features(reference):
- Characteristic pain: sudden onset, persistent, and severe epigastric pain that radiates to the back.
- Elevated serum lipase or amylase (at least three times the upper limit of normal).
- Characteristic findings of acute pancreatitis in abdominal imaging (contrast-enhanced CT, MRI, or abdominal ultrasonography).
7. Treatment of pancreatitis after gallbladder removal.
The treatment of pancreatitis after gallbladder removal has two main targets:
- Treatment of the inflammation itself (similar to the treatment of classic acute pancreatitis).
- Defining and eliminating the cause of pancreatitis recurrence after gallbladder removal (such as missed stone, alcohol, medications, etc.).
The treatment of acute pancreatitis includes (reference):
- Most cases of acute pancreatitis require hospital admission (severe cases may require admission and management in the intensive care unit).
- Aggressive intravenous fluids.
- Pain control (with analgesics sicuas opioid analgesics).
- Soft diet.
- Antibiotics.
- Management of complications such as intraabdominal collections, bleeding, or abscesses may require surgery.
8. When to see a doctor after gallbladder removal (warning symptoms of pancreatitis).
Warning symptoms of pancreatitis after gallbladder removal include:
- Persistent severe pain in the upper central abdomen (epigastric pain).
- Epigastric pain that radiates to the back.
- Epigastric pain partially improves when you sit up or lean forward.
- Severe nausea and vomiting after gallbladder removal.
- Fever.
- Severe tenderness in the upper stomach area.
- Difficulty breathing (shortness of breath).
- Signs of dehydration (extreme thirst, concentrated little urine, dry mouth, lack of tears and saliva, etc.).
- Confusion or coma.
9. Does gallbladder removal increase the risk of pancreatitis?
Gallbladder removal doesn’t increase the risk of pancreatitis. Moreover, the risk of pancreatitis dramatically decreases after gallbladder removal surgery.
Cholecystectomy surgery removes the gallstone-containing gallbladder, which, in turn, prevents future gallstone pancreatitis.
- Evidence-based
- Written by a doctor.











