6 Problems After Gallbladder Removal (Years Later)
Our content is not intended nor recommended as a substitute for medical advice by your doctor. Use for informational purposes only.
Welcome to oh-mygut.com. Dr. Farahat here.
If you are having digestive issues or gallbladder problems for months or years after gallbladder removal, it may be due to an intrinsic gallbladder problem or may be due to another digestive issue.
In this in-depth article, I’ve combined the most common causes of such gallbladder problems and how to deal with them
Key Facts:
- Problems after gallbladder removal may reappear after (or persist for) years. They are not uncommon and are related to various biliary and non-biliary conditions.
- Common problems include postcholecystectomy syndrome (biliary pain), digestive issues (such as bloating and diarrhea), development of a new stone, liver problems, and a slightly higher risk of some cancers such as colon cancer.
- These symptoms may be caused by various conditions, such as:
- Biliary and non-biliary problems.
- Gallbladder or cystic duct remnants.
- Denovo gallstone formation.
- Bile acid diarrhea.
- Bile reflux.
- Bile duct strictures.
- Adhesions.
- Slightly higher risk of cancer.
1 . Pain and digestive Issues after gallbladder removal (Post-cholecystectomy Syndrome)
About 10% of patients may suffer from persistent or re-appearance abdominal pain after gallbladder removal. In some cases, the pain may persist (or reappear) for years after gallbladder removal.
This condition is called (postcholecystectomy syndrome). And it the term is used to describe biliary colic, right upper abdominal pain, or diffuse upper abdominal pain similar to the pain experienced before gallbladder removal.
Also, the postcholecystectomy syndrome may involve other abdominal symptoms such as diarrhea, bloating, etc.
So, It is a diverse disease. And it can occur in one of three patterns:
- Temporary (for a few weeks or months after gallbladder removal).
- Persistent (for years after the operation, but it eventually ends.
- Lifelong (continues through the lifetime).
Also, the postcholecystectomy syndrome may be:
- A continuation of the symptoms experienced before the gallbladder removal.
- Development of new symptoms (either immediately or years after gallbladder removal).
From my experience as a gastroenterologist, postcholecystectomy syndrome is a term that includes a diversity of conditions (causes) and symptom patterns.
Interestingly, the most common cause of gallbladder-like pain and digestive issues (bloating, colics, diarrhea, nausea, etc.) years after the operations is unrelated to the biliary system.
Studies estimate that at least 50% of the cases of post-cholecystectomy syndrome are unrelated to the biliary system (reference).
The table below summarizes the most common causes of non-biliary that mimic gallbladder problems (even years after its removal) (reference).

The most common causes that can mimic gallbladder pain years after cholecystectomy are:
- Reflux esophagitis (gastrointestinal reflux disease), especially when the cause is a hiatal hernia.
- Peptic ulcer disease pain.
- Irritable bowel syndrome.
- Chronic pancreatitis (especially in patients with chronic alcoholism).
How can you figure out non-biliary causes?
The main feature of all these conditions is that the pain is not typical gallbladder pain (biliary colic).
Gallbladder pain has characteristic features that differentiate it from other causes of abdominal pain.
The table below illustrates all the features of biliary colic (true gallbladder pain).
| Biliary colic (Uncomplicated gallstone). | Description |
| 1. Site | Usually, The right upper quadrant of your abdomen. |
| 2. Spread | – The pain may spread to the back of the right shoulder. – Also, it spreads to the epigastric area. |
| 3. Character | Constant builds up then disappears gradually. |
| 4. Duration | At least 30 minutes. It may last up to 6 hours. |
| 5. Relation to food | – Triggered by foods (especially fatty food and large meals. – However, it can start spontaneously. |
| 6. NOT related to: | Movement, bowel movements, or the passage of flatus. |
| 7. Nausea | Often Present, severe. |
| 8- Commonly associated symptoms | Vomiting, sweating during the attack. |
| 9. Unusual symptoms. | – Heartburn and chest pain. – Bloating, fullness. – Early satiety. – Isolated epigastric pain. |
| 10. Symptoms NOT associated: | – Fever. – Jaundice. – Prolonged pain for more than 6 hours. – Extreme tenderness over the gallbladder (Murphy’s sign). – Vomiting of blood, blackish stool (PUD). |
Other conditions that may mimic gallbladder pain years after gallbladder removal:
- Reflux esophagitis (acid reflux or GERD)
The main symptoms are heartburn (burning chest sensation), regurgitation of food or acidic substances, nausea, vomiting, and upper abdominal pain. - Peptic ulcer disease pain:
Peptic ulcer disease pain is central (epigastric), related to meals, burning, or gnawing, and it is often more prolonged than gallbladder pain. - Irritable bowel syndrome.
Irritable bowel syndrome is often diffuse colicky abdominal pain that comes and goes in attacks. It can be localized in the upper abdomen. Also, the pain is often relieved by defecation and is associated with changes in bowel habits. Bloating is also common in IBS patients. - Chronic pancreatitis pain:
Patients with chronic pancreatitis (often due to alcoholism) may suffer from persistent or recurrent upper abdominal pain that mimics gallbladder problems. The pain is often severe and constant in the central upper abdomen and radiates to the back.
2. Gallbladder or cystic duct remnants.
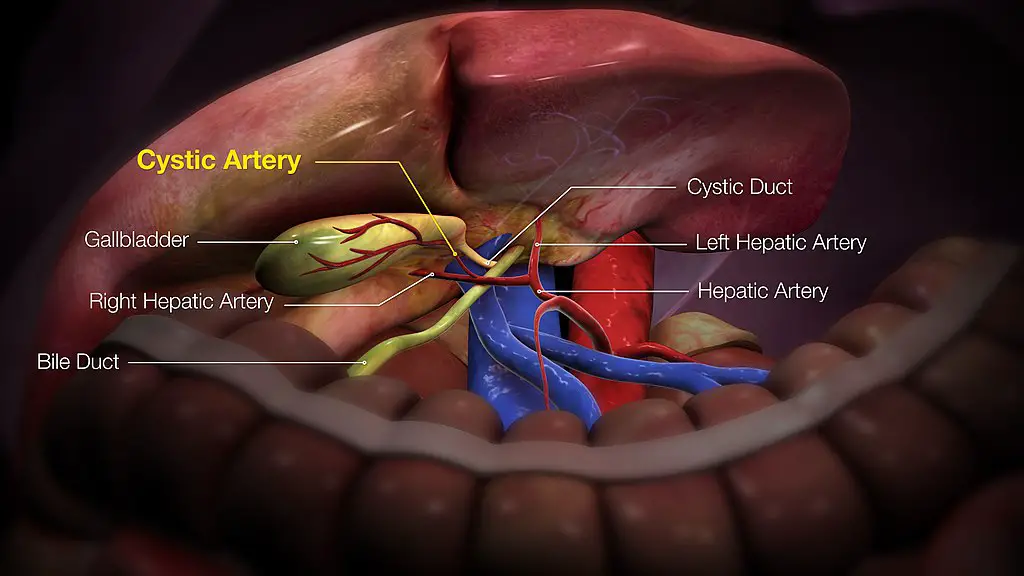
Sometimes, the surgeon doesn’t remove the gallbladder completely. In rare cases, a small part of the gallbladder or the cystic duct (short duct connecting the gallbladder to the main bile duct) is left.
As a result, a stone may form years after gallbladder removal in the gallbladder remnant or cystic duct.
Patients may present years after gallbladder removal with typical gallbladder pain (as described in the table above).
Some studies estimate that up to 13.3% of laparoscopic gallbladder removal surgery leaves a gallbladder stump.
Also, the left stump may already contain a stone. In such a case, gallbladder problems appear immediately after surgery (not after years).
Management of the condition:
The condition is easily diagnosed via abdominal ultrasound or abdominal CT.
Stone-containing gallbladder or cystic duct remnants usually require a completion surgery (reference). The remnant is removed via laparoscopic or open surgery and requires a highly skilled surgeon.
3. New (Denovo) gallstone formation.
Your gallbladder is not the only site of gallstone formation. So, you may develop a new (Denovo) gallstone years after gallbladder removal.
The new stone can form in (reference):
- The common bile duct (commonest site).
- Inside the gallbladder or cystic duct remnants.
- The right or left hepatic ducts (see the illustration in the previous section).
- Rarely, gallstones may form inside the small bile ducts inside the liver.
The risk of forming Denovo gallstones years after gallbladder removal is higher in older ages, females, pregnant women, and patients with high cholesterol levels.
Symptoms:
- New-onset typical biliary pain (as described above) appears years after gallbladder removal.
- The stone may obstruct the CBD (common bile duct), leading to jaundice, clay stools, and dark urine (obstructive jaundice).
- Moreover, the stone may obstruct the pancreatic ducts giving rise to typically acute pancreatitis (severe pain in the upper central abdomen that persists for days, referred to the back, with nausea, vomiting, and jaundice.
Diagnosis and treatment:
The condition is often diagnosed by abdominal ultrasound, MRCP (a special type of MRI that visualizes the biliary system and the pancreas).
If the stone is causing an obstruction (jaundice), you may undergo a special type of endoscopy called ERCP (Endoscopic retrograde cholangiopancreatography).
This is often definitive treatment unless a gallbladder stump may require further surgery.
4. Sphincter of Oddi dysfunction/biliary dyskinesia.
The sphincter of Oddi is a ring of muscle at the end of the common bile duct. Abnormal contractions or failure of the relaxation of the sphincter of Oddi may cause gallbladder-like pain.
The sphincter of Oddi dysfunction causes biliary-type pain and may continue for years after gallbladder removal.
Also, it can lead to pancreatic and liver problems (learn more).
Diagnosis:
- Symptoms are typical for biliary colics after gallbladder removal without other evidence of other complications (gallstones, gallbladder remnants, etc.).
- It is more common in female patients who have had their gallbladders removed.
- A special radiological test is called (quantitative hepatobiliary scintigraphy).
- ECRP (endoscopic retrograde cholangiopancreatography) with an injection of a contrast into the biliary ducts to assess the condition.
5. Secondary Bile acid diarrhea (BAD).
Bile acid diarrhea (BAD) is a common and underdiagnosed condition. Bile acid diarrhea occurs when your intestine cannot handle bile acid properly.
Your gallbladder has two main functions (reference):
- First, it concentrates the bile secreted from the liver.
- On-demand secretion of bile with eating.
Removing your gallbladder leads to the continuous flow of the secreted bile into your intestine regardless of eating. The secreted bile is also not concentrated enough.
Loss of the normal physiology of bile storage and concentration is a major contributor to gallbladder problems which may last for years.
Continuous bile flow (loss of gallbladder storage function) may lead to bile acid malabsorption and bile reflux problems.
Bile acid diarrhea (BAD) is known for its characteristic severe urgency and can present as explosive diarrhea after eating.
Interestingly, several studies stated that about 50% of IBS with diarrhea (IBS-D) patients have underlying BAD. (reference 1, reference 2).
Also, Secondary bile acid diarrhea can occur after gallbladder removal.
The symptoms of Bile acid diarrhea include:
- Diarrhea: is often triggered by eating fatty foods.
- Diarrhea can be chronic or occasional.
- Extreme and sudden urgency (explosive diarrhea).
- It may lead to soiling accidents.
- Related to fatty meals.
- Associated with bloating and abdominal pain.
The diagnosis of Bile acid diarrhea is usually difficult and overlooked by doctors because:
- Symptoms are very similar to IBS-D and chronic idiopathic diarrhea.
- The conventional tests such as stool analysis, colonoscopy, and abdominal CT test negative for BAD.
- The BAD-specific tests are not widely available.
Cholestyramine (Questran) is a bile acid sequestrant used to treat BAD. If you experience diarrhea with urgency after the gallbladder removal, consult your doctor about the possibility of BAD.
6. Bile reflux.
Sometimes, bile can flow back into your intestine and even your esophagus, which can cause a condition called bile reflux gastritis (reference).
This may lead to symptoms such as upper abdominal pain, heartburn, nausea, vomiting of greenish or yellowish fluid, cough, hoarseness, bloating, and gas.
It’s important to note that bile reflux gastritis may not respond to traditional treatments like antacids, H2 blockers, or proton pump inhibitors. Your doctor can diagnose bile reflux by visualizing bile in your stomach or esophagus through endoscopy or testing the acidity of your gastric or esophageal contents.
The good news is that there is a drug called Ursodeoxycholic acid, along with lifestyle modifications, that can help treat bile reflux gastritis. So, if you’re experiencing these symptoms after gallbladder removal, talk to your doctor about your options.
7. Bile duct strictures.
Bile duct strictures are narrowing in the bile ducts, making it difficult for bile to pass from the liver to the intestine.
Gallbladder surgery is one of the common causes of bile duct strictures. In many cases, strictures develop years later after gallbladder removal (reference).
Bile strictures can also lead to the formation of Denovo gallstones in the parts of the bile duct before the stricture.
Patients with bile duct stricture present with typical biliary colics with jaundice, clay stools, and dark urine.
The diagnosis of bile duct stricture requires MRCP (MRI with contrast to visualize the biliary system) or ERCP (endoscopic retrograde cholangiopancreatography).
Bile duct strictures are treated by passing a stent (via ERCP) to bypass the narrowing and allow the free passage of bile.
8. Post-cholecystectomy adhesions.
Adhesions at the site of gallbladder attachment to the liver (the gallbladder bed) or surrounding structures are common after gallbladder removal.
For example, One study found that the rate of adhesions after laparoscopic cholecystectomy is as high as 51% (reference).
Most cases of adhesions are often due to severe acute cholecystitis or complicated gallbladder surgeries (gallbladder abscess, perforation, etc.).
Patients with abdominal adhesions after gallbladder removal may continue to suffer from pain and digestive issues for years after the operation.
The pain is often vague and intermittent. Chronic for years, occurring in the upper right abdomen, may become diffuse.
9. Increased risk of cancer
While some studies have shown a slight increase in risk, the overall risk is still considered to be relatively low.
For example, a 2022 nationwide Korean study found that patients who underwent gallbladder removal are at a slightly higher risk of cancer (particularly colon, pancreas, liver cancers, and leukemias). Patients with cholecystectomy had a 1.19 times higher risk of cancer compared to those who didn’t remove their gallbladder.
It’s important to remember that the benefits of gallbladder removal surgery often outweigh the potential risks. However, you can take steps to reduce your risk of colorectal cancer, such as maintaining a healthy lifestyle and getting regular screenings. If you have any concerns about your health, don’t hesitate to talk to your doctor. They can provide you with more information and guidance on how to stay healthy.
FAQs about gallbladder problems years after cholecystectomy:
1. What is the most common cause of pain where the gallbladder was removed years ago?
The most common cause of pain after years of gallbladder removal is a persistent post-cholecystectomy syndrome. Post-cholecystectomy syndrome symptoms often include pain and other digestive issues such as bloating, diarrhea, and nausea. It can be caused by biliary and non-biliary conditions.
2. What are the liver problems years after cholecystectomy?
Most liver problems after gallbladder removal typically occurs during or shortly after the surgery. Late liver problems are rare and may include intrahepatic duct stones and cholestasis due to stones or strictures in the extrahepatic bile ducts.
3. Can I develop a stone inside the liver years after gallbladder removal?
Yes, You can develop a stone inside the liver years after gallbladder surgery. The stone typically develops in the small bile ducts inside the liver and may cause various liver problems, such as liver pain and cholestasis (reference).s
- Evidence-based
- Written by a doctor.

Related Posts:
- Diarrhea After Gallbladder Removal: Causes, How Long…
- Pancreas Problems: 5 Main Conditions, Symptoms, & Signs
- Heaviness in Lower Abdomen in Non-pregnant Females:…
- Safest Gallbladder Diet after Surgery (with 60+ Recipes)
- 8 Tips To Avoid Vomiting & Nausea During Colonoscopy…
- 6 Causes of Bigger Stomach after Gallbladder Surgery…