Causes Of IBS: 9 Interesting Theories (Deep Dive).
Our content is not intended nor recommended as a substitute for medical advice by your doctor. Use for informational purposes only.
The mystery of IBS continues to baffle us.
There’s no one-size-fits-all cause for IBS, making it a complex puzzle.
So, let’s dive in together, shall we?
Understanding the specific trigger of YOUR IBS could be the first real step towards conquering it.
You and your doctor can devise the best treatment strategy based on what specifically sparked your IBS.
I’ve compiled all the research about IBS causes here, in a simplified form.
Read thoroughly, and try to figure out what sparked your IBS.
The 9 Causes Of IBS:
1- Abnormal Motility Of Your Intestine.
This is one of the oldest theories about the causes of IBS. It was suggested that abnormal movement patterns in your colon and small intestine could be the culprit behind your IBS.
Normally:
Your intestine and colon contract and relax in “waves.” These waves are synchronized. We normally don’t feel them.
A wave of contraction in your colon moves slowly downwards, followed by a wave of relaxation. Then a wave of contraction starts again and travels slowly; this helps:
- Moving the food you eat down through your intestine and colon.
- Mixing food with digestive fluids & enzymes.
- Absorption of nutrients and water.
- Defecation.
It was suggested that IBS occurs due to:
- Bowel contractions occur more frequently: For example, an IBS patient may experience about 20 contraction waves (peristalsis) instead of a normal of less than ten waves per minute. More frequent bowel movements mainly cause IBS- diarrhea.
- Contractions occur less frequently: this can increase the time food resides inside your intestine. The more time food stays in your gut; the more water is absorbed into your blood, making your stool hard. Also, more gas is produced, resulting in IBS constipation, IBS bloating, and IBS gas distension.
- Irregular bowel contractions: the abnormal direction of the wave of contraction or irregular time intervals may lead to the gut pain you feel with IBS.
Evidence and how this can be applied:
The link between abnormal motility of your intestine and your IBS exists. But research is still defective as:
- These patterns of abnormal motility don’t present in all IBS patients.
- Its relation to your symptoms is unclear. I.e., some patients may have an abnormal bowel movement but no corresponding symptoms, and others may have typical IBS symptoms, and no abnormal motility couldn’t be detected.
The abnormal bowel contractions are the basis of different antispasmodic treatments, whether prescription or over-the-counter antispasmodics like Buscopan or Peppermint oil capsules.
Also, some other drugs may modify this abnormal colon motility; for example, Immodium (Loperamide) slows down the motility of your colon and consequently relieves diarrhea.
But,
The response to these “motility drugs” is variable. So, it may be the cause in some IBS patients but not all of them.
2- Your Colon Is Over-sensitive.
Normally:
Pain is perceived from your intestine by stretch receptors and other chemical mediators. This occurs when there are an extra-amounts of gas or food (distension and bloating).
Extra gas in your colon -> more stretch of colon walls -> stimulation of stretch receptors inside your colon wall -> sends a signal to your spinal cord and brain to feel pain.
As an IBS patient, you may feel gut pain, bloating, and distension even with normal amounts of gas inside your intestine.
Normal amounts of gas in your colon -> abnormally stimulate the stretch receptor in your colon wall -> sending a false signal of distension, -> you feel pain (colics, distension, or bloating).
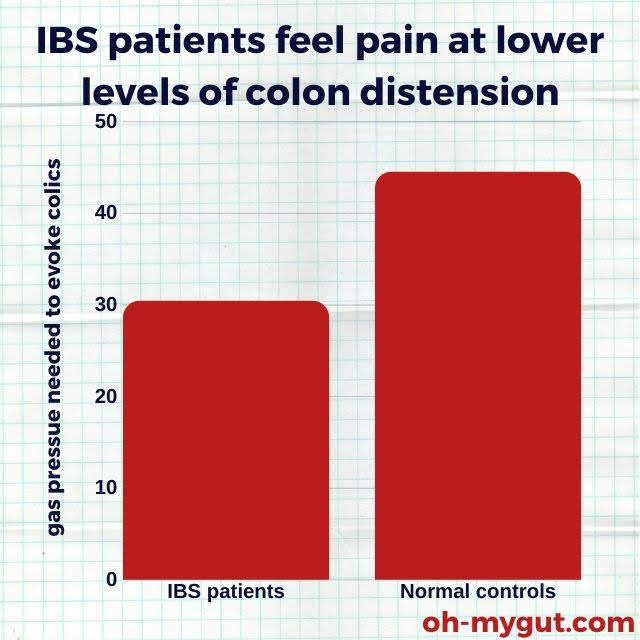
Source: This study.
Evidence & how this can be applied.
It is unclear whether the hypersensitivity of the colon is due to abnormal receptors inside your intestine or an abnormal perception of pain by your brain.
But the point is that colon hypersensitivity is frequently found in many IBS patients.
Drugs modulating pain sensations (like Tricyclic Antidepressants) may play a role in IBS relief.
3- Actual Inflammation Inside Your Colon Wall!
The widely accepted theory about irritable bowel syndrome is that it is a “functional disease.”
But there is scientific evidence that an actual inflammation could happen.
This is more common with IBS diarrhea and Post-infectious IBS.
In 2002, Dr. Törnblom and his team found a low-grade inflammation and inflammatory cells inside the colon wall of 10 patients with severe IBS.
Researchers not only found inflammatory cells (like lymphocytes and mast cells) but also found pro-inflammatory mediator proteins (cytokines.)
This may suggest that an organic cause causes IBS and is an actual disease.
4- a previous attack of gastroenteritis (post-infectious IBS)
Having an attack of enteritis raises your odds of getting IBS Up to 6 folds [REF]. This is more common with:
- Younger age.
- If you had a prolonged fever with the enteritis attack.
- Anxiety and depression.
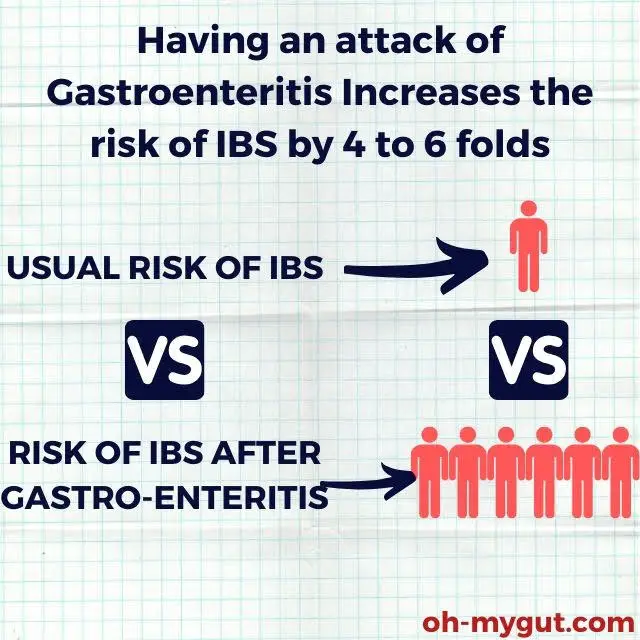
Source: This Review study
It can occur following any gut infection (Bacterial, protozoal, viral. Or helminthic).
Researchers still don’t have a clear explanation of why this occurs, but the causes may be (reference1, reference2, reference3):
- Impaired fluid and nutrient absorption following infection.
- Antibiotic use during the attack of enteritis.
- Changes in the colon wall cells (increased inflammatory cells).
If your IBS has started after a severe attack of gastroenteritis, you have to consider post-infectious IBS.
Discuss the issue with your doctor.
5- changes in the types of colon bacteria may be the real cause of IBS.
Your colon is a bustling metropolis of bacteria and microorganisms. These tiny inhabitants of your colon are not harmful but essential for your overall gut health.

These microorganisms play a crucial role in maintaining your colon health by:
- Assisting in the digestion of certain substances.
- Facilitating normal motility of your colon.
- Aiding in the absorption of specific vitamins and nutrients.
An intriguing study on the role of fecal microorganisms (Microbiota) in IBS discovered that:
- Transferring fecal microbiota from IBS patients to rats resulted in IBS-like symptoms in these rats.
- Conversely, transmitting fecal microbiota from a healthy human (not suffering from IBS) did not induce IBS symptoms in rats.
These findings may pave the way for a deeper understanding of the underlying causes of IBS.
Application1: Probiotics
Based on this hypothesis, probiotics have emerged as a promising treatment option for IBS.
Probiotics are “living microorganisms” that can counteract or reduce the changes in your colon microbiota, alleviating your IBS symptoms.
Probiotics can be derived from a single strain or multiple strains of bacteria and are available in various forms (capsules, sachets, probiotic yogurts, and others).
While some studies couldn’t detect significant changes in fecal microbiota following the administration of probiotics, the improvement of IBS symptoms with probiotics is evident.
FMT, or Fecal Microbiota Transplantation, is a fascinating application of this theory. It’s essentially a process where the fecal matter from a healthy individual is transferred to an IBS patient.
Research has indicated that FMT could be a lasting solution for IBS, but the results are still inconclusive and ongoing trials are needed.
FMT is already a recognized treatment for certain medical conditions, such as “Clostridium difficile infections.”” However, its use in treating IBS is still experimental.
6- The Impact of Bacterial Overgrowth (Could SIBO Be Behind Your IBS?)
[SIBO= Small Intestinal Bacterial Over Growth].
In the previous section, we delved into how changes in your gut’s microorganisms could be the root cause of your IBS.
But what about the microorganisms that are already present in your gut?
What if they started to act out?
Bacterial overgrowth is when the naturally occurring microorganisms in your intestine multiply beyond normal levels.
This overgrowth can have negative effects on your intestine. The excess microorganisms may produce abundant waste, such as gases or toxins. This unwanted gas and waste could be the culprits behind symptoms like distension and colic.
Small Intestinal Bacterial Overgrowth (SIBO) has been linked to IBS, but the research is mixed:[REF | REF |REF]
- There’s evidence suggesting that eliminating this bacterial overgrowth with antibiotics can lead to an improvement in IBS symptoms.
- However, another study found that SIBO isn’t inconsistent in all IBS patients. In this study, SIBO was detected in only 4% of IBS patients (the same percentage as in the healthy individuals included).
What’s the takeaway?
The connection between SIBO and IBS is still tenuous. However, eradicating bacterial overgrowth has been shown to alleviate many IBS symptoms.
For instance, a gut antibiotic called Rifaximin (Xifaxan) has been approved for treating IBS diarrhea with promising results.
7- The Role of Food Allergies:
Could your diet be triggering your IBS?
Numerous studies have explored the impact of food on IBS, and as is often the case, the evidence is mixed.
For instance, one study found that people with food allergies (identified by skin tests) are likelier to have IBS than those without IBS.
However, another study concluded that foods that tested positive by skin test didn’t necessarily induce IBS attacks.
Here are the two most commonly implicated food triggers for IBS:
A- Carbohydrates:
FODMAPs are types of carbohydrates (short-chain sugars) that are often the main culprits behind IBS symptoms. When these substances enter your gut, they are quickly fermented, producing excess gas and triggering IBS symptoms.
Limiting FODMAPs is one of the most effective strategies for managing your IBS symptoms.
FODMAP stands for “Fermentable Oligo, Di, Monosaccharides, And Polyols.”
Fermentable: This refers to gut bacteria breaking them down, producing a lot of gas.
Oligosaccharides: These are compounds called fructans and galacto-saccharides found in wheat, barley, rye, onion, garlic, and legumes.
Disaccharides: This term refers to fructose sugar in milk, ice cream, custard, and yogurt.
Monosaccharides: This refers to free fructose found in apples, pears, mangoes, cherries, watermelon, asparagus, sugar snap peas, honey, and high-fructose corn syrup.
And
Polyols: These are substances called sorbitol, mannitol, xylitol, and maltitol found in certain fruits like apples and watermelon and in artificial sweeteners like artificially sweetened gum and alcohol.
B- Gluten:
Gluten is a protein found in wheat and barley. Some people have severe gluten intolerance, a condition known as celiac disease.
Individuals with celiac disease typically experience chronic diarrhea, weight loss, and anemia.
Some studies have suggested that mild or hidden gluten sensitivity may be present in IBS patients. [REF | REF]
You may find that your symptoms improve after eliminating gluten from your diet. Additionally, we (as doctors) may need to test for celiac disease if you have IBS (especially IBS-diarrhea).
8- The Brain-Gut Connection (Stress):
Stress is a formidable adversary when it comes to IBS.
One of the most frequently proposed causes of IBS is psychological dysfunction, specifically, a disruption in the brain-gut axis.
Your colon houses local nerve clusters known as the “myenteric plexus.””
This myenteric plexus functions as a localized gut-brain linked to our central brain.
Psychological stress can prompt the brain to send irregular signals to your gut, leading to pain and changes in bowel movements (diarrhea or constipation).
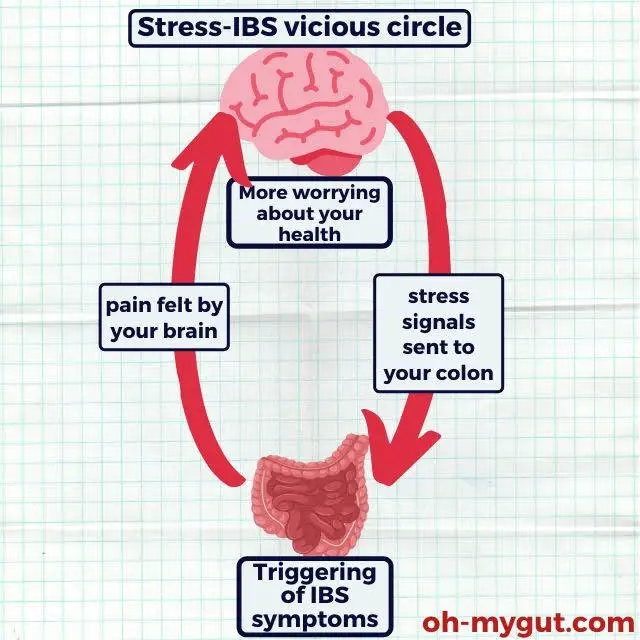
The most common psychological conditions that could potentially trigger IBS include:
- Everyday stressors such as work, exams, and so on.
- Major life stressors like the loss of a loved one.
- Depression.
- Phobias, such as the fear of contracting a serious illness (a common concern I often encounter with my patients).
9- The Role of Genetics in IBS!
If a family member has IBS, your risk of developing the condition may be slightly elevated.
While the link isn’t particularly strong, some studies suggest that genetic factors could play a role in IBS.
For instance:
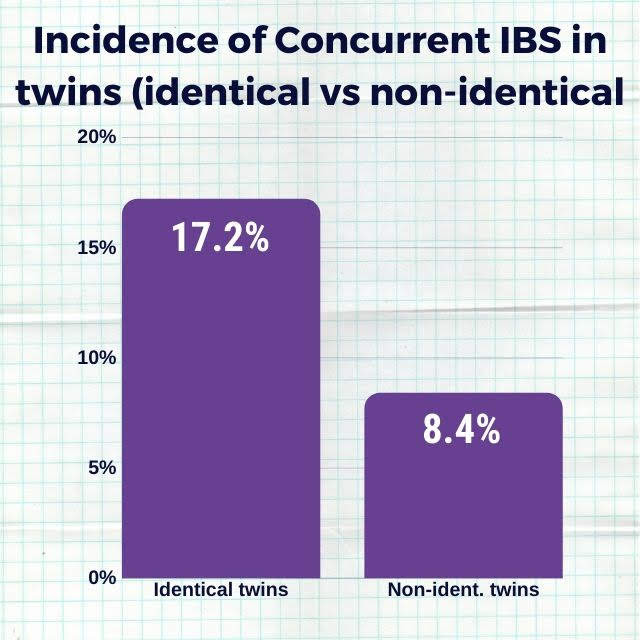
An intriguing study compared the prevalence of IBS in identical and non-identical twins.
Source: This study
The researchers discovered that identical twins (who share the same genes) were more likely to have IBS than non-identical twins.
My Take on the Causes of IBS:
There’s a wealth of research on the potential causes of IBS, but no single cause can be universally applied to all patients.
In my view, each IBS patient has their own unique set of circumstances. Your specific cause of IBS may shape your treatment plan.
Gaining a deeper understanding of the particular cause of your IBS can empower you to make informed decisions about your condition.
Always engage in open discussions about the true cause of your IBS with your doctor.
FAQs:
What causes bloating with IBS?
A variety of factors can cause IBS-related bloating:
-
Diet: Certain foods are known to cause gas and bloating. These include beans, lentils, broccoli, cabbage, onions, and carbonated drinks. Foods high in fat can also slow down digestion, leading to bloating.
-
Gut bacteria imbalance: An imbalance in the gut microbiota can produce excessive gas, resulting in bloating. This is often seen in conditions like Small Intestinal Bacterial Overgrowth (SIBO).
-
Poor digestion: If your body has trouble digesting certain types of food (like lactose or gluten), it can lead to bloating.
-
FODMAPs: These are types of carbohydrates that some people find hard to digest. They can cause excessive gas and bloating in some individuals.
-
Stress and anxiety can affect gut function and lead to symptoms like bloating.
-
Altered gut motility: In IBS, the speed at which food passes through the gut can be faster or slower than normal. Both can lead to bloating – fast transit can cause gas production, while slow transit can cause constipation and bloating.
Remember, it’s always best to discuss your symptoms with a healthcare provider to get a proper diagnosis and treatment plan.
What causes IBS-C?
IBS-C, or Irritable Bowel Syndrome with constipation, is a subtype of IBS characterized by abdominal pain and constipation. The exact cause is unknown, but several factors are thought to contribute:
-
Altered gut motility: In IBS-C, the movement of the intestines can be slower than normal, leading to constipation.
-
Brain-gut interaction: Stress and other psychological factors can affect the communication between the brain and the gut, leading to changes in bowel movements and pain perception.
-
Gut sensitivity: People with IBS-C often have an increased sensitivity to pain resulting from bloating and bowel movements.
-
Diet: Low-fiber diets can contribute to constipation.
-
Gut bacteria imbalance: Changes in the gut microbiota can also play a role in IBS-C.
What are the common causes of IBS Flare-ups?
IBS flare-ups, or periods when symptoms become worse, can be triggered by a variety of factors:
-
Diet: Certain foods, especially those high in fat, spicy foods, or certain carbohydrates known as FODMAPs, can trigger an IBS flare-up.
-
Stress: High-stress levels can exacerbate IBS symptoms.
-
Hormonal changes: Some women find their IBS symptoms worse during their menstrual periods, suggesting hormonal changes may play a role.
-
Medications: Certain drugs, including antibiotics, can trigger an IBS flare-up.
-
Gastroenteritis: Gastroenteritis or “stomach flu” can lead to a temporary flare-up of IBS symptoms.
What causes cyclical IBS?
Cyclical IBS refers to the pattern where IBS symptoms come and go over time. The exact cause of this pattern is not well understood, but it may be related to the following factors:
-
Dietary changes: Variations in diet can lead to periods of symptom relief followed by flare-ups.
-
Stress and anxiety: These can have a cyclical nature and can therefore lead to cyclical IBS symptoms.
-
Hormonal fluctuations: The menstrual cycle can cause cyclical changes in IBS symptoms in women.
-
Gut microbiota changes: The balance of bacteria in the gut can change over time, leading to cyclical IBS symptoms.
- Evidence-based
- Written by a doctor.