Pancreatic diarrhea: 7 Facts about its Causes, Symptoms, & Treatments.
Our content is not intended nor recommended as a substitute for medical advice by your doctor. Use for informational purposes only.
1. Diarrhea occurs only after the pancreas loses >90% of its function.
Your pancreas secrets about 1.5 liters of digestive juice rich in digestive enzymes.
These pancreatic enzymes help you digest different food components. Examples:
- Pancreatic lipase: helps fat digestion (aided by bile secreted from the liver).
- Pancreatic amylase: helps carbohydrate digestion.
- Pancreatic Protease helps protein digestion.
When the pancreas fails (mainly due to chronic pancreatitis), these enzymes are not released sufficiently, leading to malabsorption.
Fat malabsorption often produces characteristic pancreatic diarrhea or steatorrhea (foul, bulky, offensive, and grayish or yellow stool).
The extensive pancreatic damage leading to pancreatic diarrhea (steatorrhea) is often called (Exocrine Pancreatic Insufficiency or EPI).
2. Chronic pancreatitis is the most common cause of pancreatic diarrhea.
As we mentioned above, the pancreas must be profoundly destroyed for diarrhea to occur. This extensive pancreatic tissue damage often results from a chronic pancreatic disease that replaces the healthy parts of the pancreas with fibrous tissue.
Roughly one in every 2000 persons suffers from chronic pancreatitis and subsequent pancreatic diarrhea (reference).
Chronic pancreatitis can be caused by a wide variety of conditions and risk factors, most commonly (reference):
- Alcohol abuse.
- Smoking.
- Increased blood triglycerides (lipids).
- Genetic mutations may also play a role.
- Diabetes mellitus.
- Chronic renal failure.
- Hypercalcemia.
- Some medications.
- Severe ischemia to the pancreas as during major surgeries like open heart operations.
- Autoimmune pancreatitis (your immune system attacks your own pancreas).
- Numerous cases of chronic pancreatitis are idiopathic, meaning there is no known cause.
Symptoms of chronic pancreatitis:
- The most frequent symptom is abdominal pain (epigastric pain), which typically radiates to the back and is felt in the upper central stomach region.
- The abdominal pain increases when you lie down and often increases after eating.
- Pancreatic diarrhea (steatorrhea).
- Many cases are asymptomatic (no diarrhea and no abdominal pain).
- Weight loss.
- Osteoporosis and easy fractures.
- Chronic fatigue.
- Other signs of malabsorption and vitamin deficiencies such as headache, pallor, skin scales or rashes, etc.
- Recurrent or persistent nausea or vomiting.
3. Other causes of pancreatic diarrhea (Exocrine pancreatic insufficiency).
A. Cystic fibrosis.
It is a rare genetic disease that leads to chronic respiratory and pancreatic problems. Pancreatic diarrhea is caused by progressive pancreatic damage that develops in 80% of cystic fibrosis patients.
B. Extensive Acute Pancreatitis.
Acute pancreatitis is a dangerous condition where the pancreas quickly becomes inflamed.
When a person has acute pancreatitis, enzymes in the pancreas may digest the pancreas itself. This is called necrosis.
When the pancreas
C. Pancreatic cancer.
Patients with pancreatic cancer (especially pancreatic adenocarcinoma) may experience pancreatic diarrhea. Diarrhea typically occurs as a result of obstruction of the pancreatic duct by the tumor or due to extensive damage to the pancreas.
D. pancreatic duct obstruction.
If a stone or tumor blocks the pancreatic duct or the opening of the duct in the duodenum, pancreatic enzymes can’t get to the digestive system. This can cause pancreatitis and diarrhea.
E. Certain digestive system surgeries.
The delivery of pancreatic juice to the digestive system and the physiology of the bowels may be disrupted by certain surgeries, resulting in pancreatic diarrhea. Examples include gastrectomy, gastric bypass surgery, and extensive small intestinal resection.
F. Others.
Pancreatic diarrhea can also result from (reference):
- Benign pancreatic tumors.
- Periampullary tumor.
- Decreased endogenous lipase stimulation and production.
- Celiac disease.
- Crohn’s disease.
- Shwachman-Diamond syndrome.
- Motility disorders.
4. Pancreatic diarrhea is typically fatty and offensive.
The main cause of diarrhea with pancreatitis is the malabsorption of fats. When fat is present in excess inside the gut, it leads to bulky, offensive diarrhea.
Here are the characteristics of pancreatic diarrhea:
- Loose or watery in consistency.
- Bulky (large volume).
- Offensive or fishy-smelling.
- Light brown, yellowish, or grey in color.
- Oily (greasy) or fatty.
- Often floats on the toilet water.
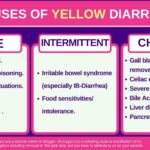
5. Many diseases may mimic pancreatic diarrhea.
Fatty or greasy diarrhea is not specific to pancreatic diarrhea. Many other diseases may cause similar stool changes.
Common mimics of pancreatic diarrhea include:
- Celiac disease: a common disease affecting about 1% of the world population. It causes severe intestinal inflammation and malabsorption after eating gluten (found in wheat, rye, and barley).
- Lactose intolerance is a very common form of food intolerance where your intestine cannot digest lactose found in milk and other dairy products.
- Small intestinal Bacterial Overgrowth (SIBO).
- Cystic fibrosis.
- Zolligner ellsion syndrome.
- Biliary obstruction (bile helps the pancreas with fat digestion).
- Whipple disease is a rare bacterial infection of the digestive system that affects how your body breaks down carbohydrates and fat.
- Giardiasis: a protozoal infection that damages the lining of the intestine and leads to fat malabsorption and yellow, offensive diarrhea.
6. How doctors diagnose pancreatic diarrhea.
The diagnosis of pancreatic diarrhea is often made by:
- Evaluation of the fat quantities in your stool (fecal fat or 72-hour fecal fat excretion test).
- Evaluation of other nutritional deficiencies
- Evidence of pancreatic damage in imaging (abdominal ultrasound, CT, or MRI).
- Fecal elastase levels.
- Stimulatory testing for the pancreatic function (administering secretin hormone to stimulate the pancreas and then collecting the pancreatic juice (via a tube inserted into the duodenum) to measure its function.
- Your doctor will also have to exclude other causes of fatty diarrhea, such as infections, celiac disease, etc.
- Nutritional assessment for nutrient deficiency is also required, such as serum vitamin D, B12, serum retinol, etc.
7. Pancreatic diarrhea treatments.
The following are some of the best remedies for pancreatic diarrhea (exocrine pancreatic insufficiency):
- Pancreatic enzyme supplements, which primarily contain lipase enzymes, are the main treatment for pancreatic diarrhea.
- Avoiding alcohol and smoking.
- Frequently eat smaller meals.
- As much as possible, maintain a normal diet and DON’T restrict fat.
- Eat a diet rich in fiber.
- Suppression of stomach acid (a proton pump inhibitor or H2 blockers) may also be helpful.
- Your doctor will often refer you to a dietician to evaluate you for any nutritional deficiency. Vitamin and micronutrient levels and bone scans are often needed. Vitamin and nutrient supplements may be needed.
- Evidence-based
- Written by a doctor.