Amoebiasis Stool: Color, Smell, & Characteristics
Our content is not intended nor recommended as a substitute for medical advice by your doctor. Use for informational purposes only.
Entamoeba histolytica is a common protozoal organism famous for amoebic dysentery. Symptomatic intestinal amoebiasis leads to profound stool changes such as mucus and bloody stools.
However, most amoebiasis infections are asymptomatic with normal stool (no stool changes).
Areas with high entamoeba infection include:
- Africa.
- India.
- Mexico.
- And some parts of central and south America.
In the united states, Entamoeba infection is responsible for many cases of diarrhea and dysentery in people who travel abroad (traveler’s diarrhea).
Fortunately, most cases of amoebic dysentery are asymptomatic or mild. Dysentery and stool changes are often mild than bacterial dysentery (bacillary dysentery).
Table of Contents
1. Amoebiasis stool colors.
Symptomatic amoebiasis is present with yellow-colored stool with mucus and may be red blood (dysentery).
The amebic following are various stool colors with the amoeba.
A. Reddish (bloody) stool.
Symptomatic intestinal amoebiasis often presents with mild to moderate dysentery. The term “dysentery” refers to the presence of blood and mucus in stool with the recurrent urge to poop.
The amoebic stool often appears brown or yellowish with reddish spots or chunks of bloody mucus. In severe cases, the poop may turn entirely red due to severe bleeding.
Bloody diarrhea (red amebiasis stool color) occurs in 94 to 100% of the cases (reference).
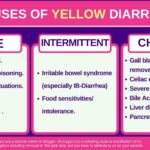
B. Yellowish diarrhea.
Some cases of amoebic diarrhea develop diarrhea without blood. In such cases, the amoebic stool appears yellowish in color and watery. Mucus (white chunks of fuzzy material) is often present.
Amoebic diarrhea typically starts gradually and continues for weeks.
C. Light-brown to yellow stool with white fuzzy mucus.
In milder cases of amoebiasis, the stool may appear loose, light brown, or dark yellow. In such cases, the symptoms (diarrhea) are often very mild, and the stool may or may not contain white mucus.
D. Brown-colored stools (Normal stools).
Not all cases of amoebiasis are symptomatic. 90% of Entamoeba histolytica infections pass without any symptoms or stool color changes (reference).
The stool appears normal in consistency and color (brown) in such cases. However, the entamoeba cysts or trophozoites can
E. Amoebiasis green stool.
In some cases of amoebiasis with severe diarrhea, diarrhea may turn green due to the passage of unchanged bilirubin giving the stool green color.
However, green stool is not characteristic of amoebiasis, and it can occur with any form of severe diarrhea as well as green-colored foods and drinks (such as green leafy vegetables).
Learn more about the causes of green stool.
2. Amoebiasis stool smell.
In patients with amoebic dysentery, the stool smell is often more offensive and foul than normal. Some may describe it as fishy or sulfur-smelling.
However, no characteristic smell differentiated amoebiasis from other gut infections. The abnormally offensive stool is a sign of either malabsorption or infection in general (not specific to amoebiasis).
3. Chronic amoebiasis stool changes (rare).
Chronic amoebiasis is an uncommon condition occurring when amoebiasis symptoms last for years. It starts as a mild infection and lasts for years.
The condition is often misdiagnosed as irritable bowel syndrome (chronic abdominal pain, recurrent diarrhea, and mucus in stool).
The stool in patients with chronic amoebiasis is often loose or watery, light-brown to yellowish in color. It may or may not contain mucus and blood. However, dysentery is often absent (no bloody stools).
Other symptoms suggestive of chronic amoebiasis include:
- Chronic diarrhea.
- Chronic mucus in stool.
- Weight loss.
- Chronic abdominal pain.
4. Other amoebiasis stool characteristics.
Other stool changes with clinical amoebiasis (besides color and smell changes) may include:
- Mucus-only stools (rare).
- Blackish stools or black chunks in poop (due to fulminant colitis and blackish blood in stools).
- Tenesmus: A persistent urge to poop and a sense of incomplete evacuation.
- Floating stools.
- The fuzzy or fluffy coating on the stool is due to mucus content.
5. How to suspect amoebiasis (symptoms).
Typical symptoms of intestinal amoebiasis include:
- History of traveling abroad or contact with an infected person or contaminated food.
- Gradual onset of symptoms (over days or weeks)
- The stool changes range from mild diarrhea to dysentery with bloody stool.
- The following are common symptoms and their frequencies:
- Abdominal pain (cramps): 12-80%
- Diarrhea: 94-100%
- Bloody stool: 94-100%.
- Weight loss: 50%
- Fever: 40%
- Other symptoms include anorexia, mucus in stool, nausea, and vomiting.
- Complications may also develop intestinal perforation (fulminant colitis) or amoebic liver abscess.
Diagnosis of amoebic dysentery is made by:
- Stool analysis (visualizing the organism or its cysts under the microscope).
- Stool antigen tests.
- PCR (Polymerase Chain Reaction) tests.
- Blood tests (serum antibodies) are less helpful as they cannot distinguish between current and past infections.
- Abdominal ultrasound or CT may be helpful if complications or extra-intestinal spread is suspected.
6. Mimics of amoebiasis stool.
Other mimics of amoebiasis stool (diarrhea or dysentery with blood and mucus) include:
- Bacillary dysentery: caused by shigella bacteria.
- Other bacterial infections and food poisoning.
- Inflammatory bowel disease.
- Sexually-transmitted diseases.
- Antibiotic-associated colitis.
- Radiation colitis.
- Diversion colitis.
- Colorectal cancers.
- Irritable bowel syndrome.
- Intestinal Tuberculosis.
7. Treatment of Amoebic dysentery/diarrhea.
All amoebic infections must be treated even if there are no symptoms.
Treatment options include:
- Paromomycin antibiotics (indicated for all infections, whether symptomatic or not, it helps the elimination of entamoeba cysts to prevent future activation).
- Metronidazole (Flagyl®) antibiotic.
- Tinidazole.
- In severe cases, Broad-spectrum antibiotics may be needed.
- Evidence-based
- Written by a doctor.