What Does C. Difficile Poop Look Like?
Our content is not intended nor recommended as a substitute for medical advice by your doctor. Use for informational purposes only.
Key facts:
Poop in patients with C. difficile may be normal or watery (diarrhea). Diarrhea with C. difficile infection may look like other types of diarrhea (yellow and watery) or contain reddish or blackish blood and mucus.
- C. difficile is famous for bloody diarrhea. However, it is not the only stool change occurring with C. difficile infection.
- C. Difficile infection causes a wide range of symptoms ranging from asymptomatic carrier to fulminant colitis with complications such as toxic megacolon or perforation of the colon.
- Bloody poop is not a characteristic feature of C. difficile infection, as the infection may cause mild diarrhea without blood. Also, Bloody poop may occur due to various causes other than C. diff.
- Possible poop changes associated with C. Difficile include:
- Bloody (reddish) diarrhea.
- Watery yellow diarrhea.
- Blackish poop (melena).
- Mucus diarrhea.
- Normal poop.
1. What is clostridium difficile infection?
C. difficile is virulent bacteria that cause a severe infection of the colon. Infection with C. diff often occurs due to antibiotic use.
Antibiotics kill the beneficial bacteria residing in the colon (colon microbiota). As a result, C. diff finds a way to infect the colon.
The infection with C. difficile usually happens during antibiotic treatment or within the first two weeks after taking the antibiotics.
C. difficile produces a powerful toxin that leads to severe inflammation of the colon lining with watery or bloody diarrhea.
C. difficile infection can range from completely asymptomatic to life-threatening colon inflammation or perforation.
The treatment of C. difficile is often difficult, and about 25% of patients will have recurrent symptoms.
2. What is the spectrum of symptoms in patients with C. difficile infection?
Before describing what C. diff poop looks like, you should first learn some basic facts about the possible presentations of c. diff infection.
Not all cases of C. difficile infection cause poop changes. You may have C. difficile infection with a completely normal poop (no diarrhea, no blood or mucus in poop).
Possible presentations of C. difficile infection (reference):
A. Non-severe disease (watery diarrhea): the passage of yellow watery diarrhea (three or more motions per day) with lower abdominal pain, nausea, low-grade fever, and anorexia. ****
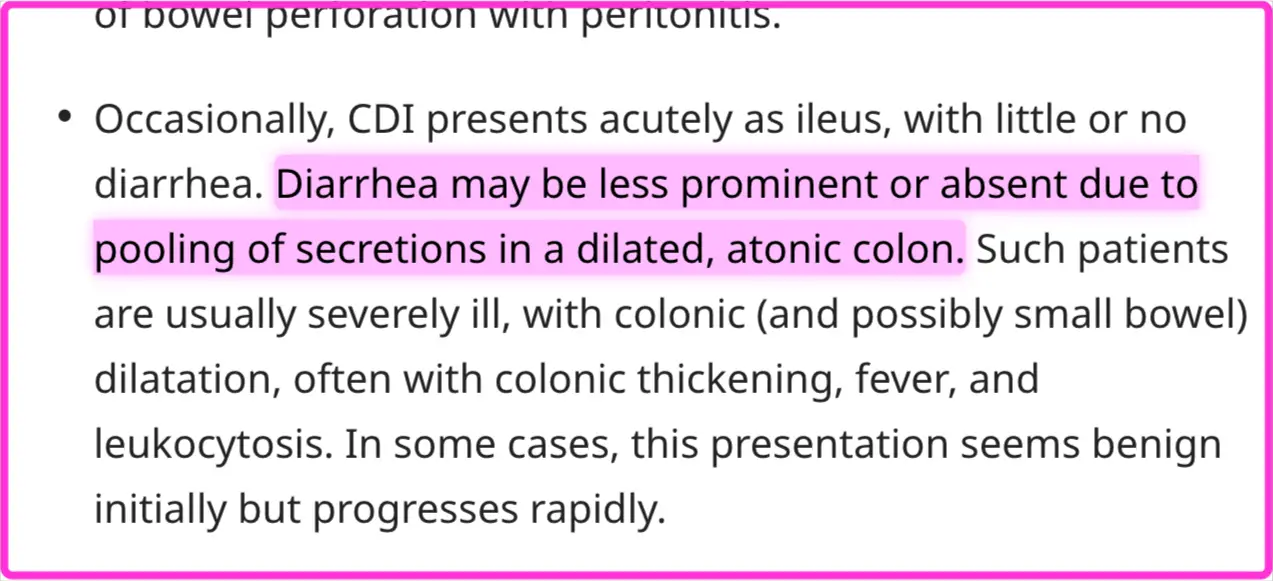
B. Severe disease (fulminant colitis): Diarrhea may or may not be severe, with blood in the stool. In some cases of severe fulminant colitis, patients may have little or no diarrhea due to the pooling of secretions in the dilated colon (toxic megacolon).
Severe CDI often causes high-grade fever, shock (hypotension), and toxic symptoms.
C. Recurrent disease: Reappearance of C. difficile symptoms two to eight weeks after its resolution. Up to 25% of patients experience recurrent C. difficile infection (reference).
D. Asymptomatic C. difficile infection (carrier): Studies found that asymptomatic clostridium difficile infection can occur in up to 20% of hospitalized patients (reference).
**E. Unusual presentations (**protein-losing enteropathy, appendicitis, Soft tissue infections, etc.).
Because C. difficile infection comes in many different presentations and clinical scenarios, we couldn’t depend on poop changes alone for its diagnosis.
In the next section, we will discuss all the possible poop changes associated with c. difficile infections, including poop consistency, color, presence of blood, etc.
3. What does C. diff poop look like?
Possible poop changes associated with C. difficile infection include:

A. Watery diarrhea.
Many patients with C. difficile infection will have non-specific watery diarrhea. This is because C. difficile doesn’t necessarily cause blood in the stool.
The C. difficile watery diarrhea is often more than three motions per day with loose or watery stool. The color of the stool is often yellowish, and it may be mixed with some mucus.
The yellow watery diarrhea resembles stomach flu diarrhea with no specific symptoms.
Associated symptoms include lower abdominal cramps, fever, anorexia, nausea, or vomiting.
B. Bloody (reddish) diarrhea.
In more severe cases of C. diff. Infection, diarrhea becomes bloody with reddish blood mixed with stool. Bloody stools are often associated with fever, severe lower abdominal pain, anorexia, and nausea.
Tenesmus (persistent urge to poop) with blood and mucus only coming out may occur in some cases when the rectum and sigmoid colon are involved.
C. Melena (black stool).
Less commonly, C. diff poop may turn black (processed blood). Also, the stool may be normal brown or yellowish with black spots.
D. Mucus diarrhea.
Sometimes, C. diff diarrhea is associated with noticeably large amounts of mucus (with or without blood) in poop. Mucus results from continuous colon and rectum inflammation with little stools and lack of bleeding.
The mucus appears as a white coating on the stool (which is often watery and yellow).
E. Normal Poop.
In many cases, C. diff infection may be present without any symptoms (carrier state). In such a case, the poop appears completely normal (well-formed and brown).
Do poop changes always reflect the severity of C. difficile infection?
The severity of diarrhea and blood in stool doesn’t reflect the severity of C. diff symptoms.
For example, patients with fulminant colitis due to C. difficile infection may develop Toxic megacolon (massive dilatation of the colon). The secretions pool in the massively dilated colon, resulting in little or no diarrhea (reference).
4. How to suspect C. difficile infection as a cause of poop changes?
Unfortunately, no specific poop changes can accurately diagnose C. difficile infection.
The suspicion of C. difficile is based on a combination of the following:
- Presence of the risk factors.
- Presence of suspicious symptoms consistent with C. diff.
- Absence of other explanatory causes.
Risk factors for C. difficile infection (reference):
- Recent antibiotic use (See the table below).
- Being older.
- Recent hospitalization.
- Severe co-morbid illnesses.
- Other (less established risk factors):
- Enteral tube feeding.
- Recent gastrointestinal surgery.
- Obesity.
- Cancer.
- Chemotherapy.
- IBD (inflammatory bowel disease).
- Liver cirrhosis.
- Hematopoietic stem cell transplantation.
- Gastric acid impression (using PPIs such as omeprazole).
The table below illustrates the common and uncommon antibiotics associated with C. difficile infection (reference).
| Frequency | Examples |
|---|---|
| Frequently associated | 1. Flourquinlones (as ciprofloxacin and levofloxacin) |
| 2. Clindamycin | |
| 3. Penicillins and combinations (broad spectrum penicillins) such as amoxicillin-clavulanate. | |
| 4. Cephalosporins (2nd, 3rd, and 4th generations). | |
| 5. Carbapenems (as imipenem and meropenem). | |
| Occasionally associated | 1. Macrolides. |
| 2. Narrow-spectrum penicillins. | |
| 3. 1st generation cephalosporins. | |
| 4. Trimethoprim-sulfamethoxazole. | |
| 5. Sulfonamides. | |
| Rarely associated | 1. Aminoglycosides. |
| 2. Tetracyclines | |
| 3. Tigecycline. | |
| 4. Chloramphenicol. | |
| 5. Metronidazole. | |
| 6. Vancomycin. |
The presence of risk factors (such as recent antibiotic use) plus unexplained diarrhea should raise suspicion about C. difficile infection.
5. How is C. difficile infection (CDI) diagnosed?
The diagnosis of CDI is based on detecting the organism or its toxin.
Common tests used to diagnose CDI include (reference):
- GDH stool antigen test.
- Toxin A and B stool tests.
- NAAT (Nucleic acid amplification test) stool test (most important test).
- Rarely used tests such as Cell culture cytotoxicity assay and selective anaerobic culture.
Based on suspicious symptoms and risk factors, your doctor often orders GDH stool antigen tests and Toxin tests:
- If both tests are positive, no further tests are required.
- In addition, your doctor will often perform a NAAT test if one is positive and the other is negative.
- Evidence-based
- Written by a doctor.