IBS or Colon Cancer: In-depth Guide to differences by GI Doctor.
Our content is not intended nor recommended as a substitute for medical advice by your doctor. Use for informational purposes only.
Quick Overview:
It’s common for us, the individuals grappling with IBS, to sometimes misconstrue our gut pain. We often end up suspecting the worst possible scenario—colon cancer. However, it’s essential not to stress too much as it may exacerbate your IBS. It would be best if you only were alarmed when you observe the following:
- Blood in your stools
- Frequent weight loss
- A sense of incomplete emptying or a mass in your rectum
- Regular vomiting
- Recurring fever of unknown origin
Abdominal pain or recurring episodes of diarrhea alone are not specific signs of colon cancer. So, it’s not something you should be excessively worried about. Interestingly, many colon cancer cases present no symptoms, necessitating regular screening.
Identifying the Difference: Colon Cancer Pain vs. IBS Pain
Is the pain associated with IBS different from that of colon cancer? This question may have crossed your mind. After digging through various research papers, it appears your abdominal pain is not the primary concern.
Studies reveal that abdominal pain as a single symptom is the least common sign of colon cancer—observed in less than 4% of cases, primarily in the later stages.
People tend to worry about abdominal pain often, but it’s not a significant concern about colon cancer—unless the pain differs from typical IBS symptoms. Pain from colon cancer is typically a dull, constant ache, usually unrelated to meals. In contrast, IBS pain is a fluctuating colicky discomfort often related to meal times.
What is the First Symptom of Colon Cancer?
The first symptom of colon cancer is usually a change in your bowel habits—diarrhea or constipation. The second most common symptom is blood in your stools, ranging from fresh red to dark red or black.
The bleeding usually begins when the cancer mass inside the colon starts to bleed. Initially, the amount of blood is small and can be easily overlooked. It’s essential to pay attention to your stool color to avoid missing this symptom.
Subtle signs of bleeding may be just dots of red or black within your stool. Other symptoms include persistent fatigue, generally due to anemia from blood loss. Some people may feel a mass inside their rectum or abdomen, which is relatively rare.
To give you a clear picture, here are the common symptoms of colon cancer, along with the percentage of cases presenting each symptom (source):
- Constipation or diarrhea: 75% of colon cancer patients (Unfortunately, diarrhea and constipation are also very common with IBS)
- Dark or bright red blood in stool: 50% of colon cancer patients
- Rectal mass: 25%
- Anemia and iron deficiency: 10%
- Isolated abdominal pain: Only 3.8%
There may also be some general symptoms not directly related to your colon, such as unexplained fever, progressive weight loss over the past few months, and nausea or loss of appetite.
Does IBS Lead to Colon Cancer?
In a nutshell, NO. Nevertheless, those with IBS-C (Irritable Bowel Syndrome with constipation predominance) may face a slightly elevated risk due to the extended presence of stool in the intestine. This allows toxins to irritate the colon lining and affect the cells along its wall.
As per the American College of Gastroenterology, the risk of colorectal cancer is associated with chronic constipation, not IBS. If you have IBS-C, you can mitigate this risk using anti-constipation agents and colon detoxes.
However, the primary issue with IBS is the potential misdiagnosis of colon cancer. In other words, while IBS doesn’t pose a risk for colon cancer, its symptoms may obscure the cancer diagnosis.
How can this issue be addressed? There are two crucial actions you should take to avoid colorectal cancer if you have IBS:
First, educate yourself more about colon cancer to assess your risk accurately.
Second, take measures to shield yourself from getting colon cancer. Continue reading as we delve into both these steps.
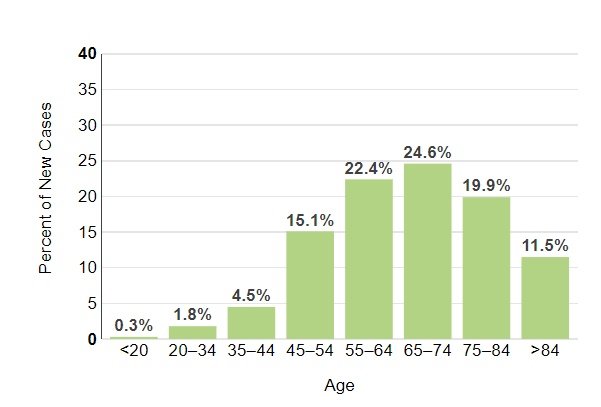
How Prevalent is Colon Cancer by Age?
Many individuals harbor fears of developing colon cancer at a young age. However, the reality is that over 90% of new colon cancer cases occur in individuals over 50.
To put things into perspective, consider the following stats:
- Age 30 to 35: Only 3 per 100,000 individuals get colon cancer.
- Age 35 to 40: 6 per 100,000 individuals.
- Age 40 to 45: 9 per 100,000 individuals.
- Age 45 to 50: 23 per 100,000 individuals.
And these numbers are way less than older age incidences. For example, people over 80 have an incidence of 500 cases for a 100000 population.
Also, only 10% of cases occurred below the age of 50.
MORE: Colon Cancer in Young Women: Sings, Risk Factors & Incidence.
The stat below shows the percentage of new cases by age.
Colon cancer Stool V.S. IBS stool: what is the difference?
The fundamental discrepancy between the stool in Irritable Bowel Syndrome (IBS) and colon cancer lies in the presence of blood. This blood can vary in color from fresh red, dark red, to even black. Remember, if you’re suffering from IBS, it’s highly unlikely to find blood in your stool.
Therefore, any occurrence of blood in your stools, irrespective of your abdominal discomfort, warrants a prompt visit to your healthcare provider. Having blood in your stool could be due to a myriad of conditions, not necessarily indicating colon cancer. The takeaway here is not to panic at the sight of blood but also not to ignore it.
More info on Mushy Stool as a Sign of Colon Cancer and Can Yellow Stool Be A Sign Of Colon Cancer?
Can Diarrhea Indicate Colon Cancer?
Diarrhea in isolation is not a specific red flag for colon cancer. It only becomes a potential sign when it occurs alongside warning signs like bloody stools, weight loss, severe nausea, and recurring fever. So, if you’re experiencing typical IBS symptoms such as abdominal pain and diarrhea, there’s no need for immediate alarm.
However, it’s essential to seek medical attention if diarrhea becomes persistent, non-responsive to common IBS medications, or is associated with the above warning signs.
Potential Triggers for Colon Cancer in IBS Patients
- Unhealthy Dietary Practices
Certain dietary habits can elevate your risk of colon cancer. These include consuming high-fat, processed foods, and having a low-fiber diet.
- Smoking and Alcohol
Studies have shown that individuals who smoke or consume alcohol more frequently have a higher risk of colon cancer.
- Obesity
Being overweight is a well-documented risk factor for various types of cancers, including colon cancer.
- Sedentary Lifestyle
An inactive lifestyle is recognized as a contributing factor to colorectal cancers. Those who ignore the significance of regular physical activity and maintaining fitness levels may face a higher risk.
- Other (Non-Modifiable) Factors
There are certain risk factors that are beyond our control, including:
◦ Advanced age. ◦ Family history of colon cancer. ◦ Pre-existing conditions like diabetes mellitus. ◦ Inflammatory bowel diseases such as Crohn’s and ulcerative colitis. ◦ Racial factors (for instance, African American race).
When Should You Get Screened for Colon Cancer?
The American Cancer Society advises everyone above the age of 45 to start screening for colon cancer. You have a choice between two types of tests:
- Stool-based tests: These involve giving a stool sample for analysis.
- Visual-based tests: These involve your healthcare provider examining your colon either through a colonoscopy or a computerized tomography (CT scan).
However, those at higher risk due to family history, obesity, or diabetes should start screening at a younger age. You should discuss with your doctor to decide on the best test for you. The key point is to ensure you get tested if necessary, regardless of the method.
IBS and Colon Cancer Prevention – What Can You Do?
1. Prevent Constipation
IBS sufferers with constipation have a higher risk of developing colon cancer. Constipation can cause toxins to linger in your colon longer, thus increasing the risk of cancer. Here’s what you can do to avoid constipation:
◦ Incorporate a high-fiber diet into your meal plan. ◦ Hydrate sufficiently every day. ◦ Include dried plums and prune juice in your diet as they’re rich in the sugar substitute sorbitol. ◦ Limit your intake of high-protein diets. ◦ Avoid bread and cereals made from refined grains – whole grains are a better option. ◦ Reduce your consumption of carbonated drinks and coffee. ◦ Limit dairy products, especially cheese.
2. Regular Screening Post 45
As mentioned earlier, start getting screened for colon cancer once you reach 45. However, start screening at an earlier age if you fall into the high-risk category due to reasons like diabetes, obesity, a family history of colon cancer, or being of African American descent. Remember to get screened every year.
3. Start a Weight Management Program if Obese
Obesity is linked to various diseases, not just cancer. Here’s how you can manage your weight:
◦ Incorporate a daily walking routine. ◦ Follow a weight-loss diet program. ◦ Try a high-fiber, low FODMAP Diet. ◦ Check out these three proven recipes for weight loss in IBS patients.
4. Stay Active
An inactive lifestyle significantly increases the risk of colon cancer. Therefore, it’s crucial to adopt a more active routine:
◦ Consider joining a gym. ◦ Get a treadmill for home use. ◦ Even light exercise at home can help; several phone apps offer home-based exercises without the need for equipment. ◦ Aim for a 30-minute walk every day.
Following these tips can dramatically improve your IBS, assist with weight loss, and protect against cancer and other diseases.
5. Quit Smoking and Limit Alcohol
If you smoke or drink alcohol, aim to cut down and eventually quit.
Related: How to Safely Consume Alcohol When You Have IBS
6. Probiotics Can Be Beneficial
Growing evidence suggests that probiotics may reduce the risk of colon cancer. Certain types of probiotics can prevent or treat colon cancer by releasing histamine, which in turn reduces inflammation and suppresses tumor progression in the colon. However, it’s crucial to choose high-quality probiotics suitable for IBS.
7. Other Protective Agents
Consider incorporating foods or supplements rich in Vitamin B6 (pyridoxine), Vitamin B9, folic acid, Calcium, vitamin D, garlic, and fish into your diet if you’re deficient. These are known to offer protection against colon cancer.
FAQs:
What are the early signs of colon cancer?
Early signs of colon cancer may include:
- Changes in bowel habits, such as diarrhea, constipation, or narrowing of the stool that lasts for more than a few days.
- A feeling that you need to have a bowel movement that is not relieved by doing so.
- Rectal bleeding or blood in the stool.
- Persistent abdominal discomfort, such as cramps, gas, or pain.
- A feeling of not being able to empty your bowel completely.
- Weakness or fatigue.
- Unexplained weight loss.
Many of these symptoms can also be caused by conditions other than colon cancer, such as infection, hemorrhoids, or irritable bowel syndrome. However, if you have any of these issues, it’s important to see your doctor.
Is abdominal pain a symptom of colon cancer?
Yes, abdominal pain can be a symptom of colon cancer. The pain is usually persistent and may be accompanied by other symptoms such as unexplained weight loss, changes in bowel habits, or blood in the stool. However, abdominal pain can be due to many different conditions, and most are not cancer. Isolated abdominal pain without other gastrointestinal symptoms is rarely due to colon cancer.
Can IBS turn into colon cancer?
No, irritable bowel syndrome (IBS) does not increase the risk of developing colon cancer. IBS is a disorder that affects the large intestine, causing symptoms like cramping, abdominal pain, bloating, gas, and diarrhea or constipation. While the symptoms can be uncomfortable and even severe, IBS does not cause changes in bowel tissue or increase your risk of colorectal cancer.
Is there a link between diet and colon cancer?
Yes, certain dietary habits are linked to an increased risk of colon cancer. These include:
- A diet low in fiber and high in fat and calories
- A diet high in red meats (such as beef, pork, lamb, or liver) and processed meats (like hot dogs and some luncheon meats)
- Cooking meats at very high temperatures (frying, broiling, or grilling) can create chemicals that might increase cancer risk.
How effective is screening for colon cancer?
Screening is effective at detecting colon cancer in its early stages when it is more likely to be curable. The type of screening test used can also prevent colon cancer by finding and removing polyps before they turn into cancer. It is estimated that routine colon cancer screening can reduce the risk of dying from the disease by about 60-70%.
How can I reduce my risk of colon cancer if I have IBS?
To reduce your risk of colon cancer if you have IBS:
- Eat a balanced diet that’s high in fiber. Include plenty of fruits, vegetables, and whole grains.
- Maintain a healthy weight and be physically active.
- Limit alcohol consumption and avoid smoking.
- Get regular screenings for colon cancer, especially if you’re over 45 or have a family history of the disease.
- Evidence-based
- Written by a doctor.