Are you experiencing constant bloating and unsure why?
Bloating is one of the most common digestive issues—and one of the hardest to manage.
Even as healthcare providers, we don’t fully understand it. The cause isn’t the same for everyone, and most of the time, it’s due to multiple factors working together.
Food, however, plays a big role. Certain foods can exacerbate bloating.
The good news? What and how you eat can make a huge difference. In fact, changing your eating habits alone may help relieve up to 90% of bloating.
In this article, you’ll learn three key things:
- The science behind bloating: because the real cure starts with understanding.
- Foods that trigger bloating—and foods that help ease it.
- Extra strategies to reduce bloating quickly.
Understanding Bloating
Bloating isn’t one thing. And if you think it’s always “too much gas,” that’s not the whole story.
I dug deep into the research on why bloating happens. There are several mechanisms, and they often overlap.
To feel better, you first need to identify your main driver(s). Then your treatment choices make sense.
P.S. You may have more than one factor.
Here’s what you need to know:
1) Gas Bloating
Gas is common, but it’s not always excessive gas. Sometimes it’s normal gas in a sensitive or crowded gut.
Where gas comes from:
- High-FODMAP foods: beans, lentils, onions, garlic, wheat, many fruits/sweeteners. These short-chain carbs feed gut bacteria → fermentation → gas.
- Swallowed air: fast eating, talking while eating, drinking through straws, carbonated drinks, gum.
- Post-meal lying down: makes it harder to burp out swallowed air.
Clues it’s gas-dominant:
- Audible stomach sounds, frequent belching or passing gas, more discomfort after high-FODMAP meals.
Quick test: run a short low-FODMAP trial (7–14 days), then systematically reintroduce.
2) Fluid Bloating (Water Retention Inside the Gut)
This is about fluid shifts, not fat gain.
Why it happens:
- Osmotic load: sugars/sugar alcohols (lactose if intolerant; sorbitol, mannitol, xylitol) pull water into the intestine.
- Salt-heavy meals: can cause temporary water retention and a “puffy” belly.
- Hormonal shifts: premenstrual phase often brings extra fluid and slowed transit.
- Malabsorption: poorly absorbed carbs increase luminal water.
Clues it’s fluid-dominant:
- Rapid “ballooning” within 1–3 hours of eating sweets or sugar-free gum/candies.
- Bloating improves overnight, returns with certain snacks.
What helps:
- Cut back on sugar alcohols, test lactose removal, moderate sodium, sip water steadily (don’t chug), and favor balanced meals over sugar hits.
3) Hypersensitive Gut (Subjective Bloating)
Your abdomen may feel very distended even when gas/volume isn’t high. This is visceral hypersensitivity—the nerves in your gut send stronger “stretch/pain” signals.
Triggers:
- IBS, stress, poor sleep, prior infections, gut–brain axis dysregulation.
Clues it’s sensitivity-dominant:
- Discomfort out of proportion to visible distention.
- Pain/anxiety cycles, symptom flares during stress.
What helps:
- Gentle low-FODMAP pattern, regular meals, peppermint oil, gut-directed breathing, walking, and—when needed—targeted gut-brain therapies.
4) Delayed Stomach Emptying (Slow Gastric Emptying)
When the stomach empties slowly, food lingers and you feel full, tight, or “stuck.”
Clues it’s gastric emptying-dominant:
- Early fullness, nausea after fatty/large meals, symptoms worse late day, relief is slow.
- More common with diabetes, hypothyroidism, certain meds (opioids, GLP-1s), and after viral illness.
What helps:
- Small, low-fat, lower-fiber meals spread across the day.
- Warm fluids (ginger tea), gentle activity after meals, and avoiding large late dinners.
5) Abdominal Wall & Diaphragm Mechanics
Sometimes the issue is how your abdominal wall and diaphragm respond to meals.
What happens:
- The diaphragm can push down while the belly pushes out—your gut volume doesn’t need to be huge to look/feel distended.
- Slouched posture compresses the abdomen and traps gas.
Clues it’s mechanics-dominant:
- Visible “end-of-day” dome belly, worse when seated or slumped; improves when you lie flat or do posture resets.
What helps:
- Eat upright, walk after meals, core and diaphragm training (box breathing), and avoid tight waistbands.
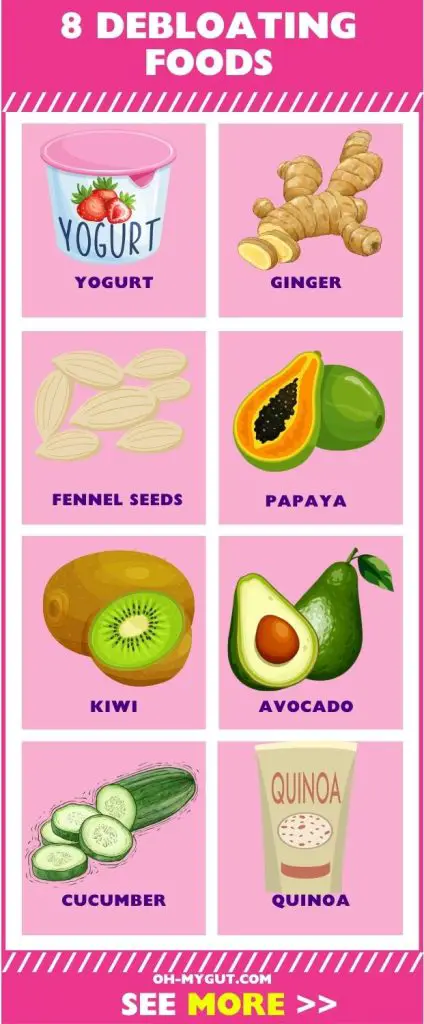
Debloating Foods
The Real Magic: Avoid Your Triggers First
- FODMAPs: Start with a short elimination (7–14 days) focusing on common triggers (wheat, onion, garlic, beans, certain fruits/sweeteners). Then re-introduce one by one to find your personal limits.
- Lactose: If dairy bloats you, try lactose-free milk/yogurt or use lactase enzyme when you want regular dairy.
- Sugar alcohols: Limit sorbitol, mannitol, xylitol, erythritol in “sugar-free” snacks and gums.
Gentle, Bloat-Friendly Choices
Ginger
- Why it helps: Supports gastric emptying and motility; settles nausea.
- How to use: Fresh ginger tea with meals, 1–2 tsp grated in stir-fries, or standardized capsules if needed.
Peppermint (Tea, Oil, or Supplements)
- Why it helps: Natural smooth-muscle relaxant; eases cramps and pressure.
- How to use: Peppermint tea after meals or enteric-coated peppermint oil 30–60 minutes before meals if cramping dominates.
Fennel Seeds
- Why it helps: Traditional carminative—reduces gas sensation and spasm.
- How to use: Light tea or chew ½–1 tsp seeds after eating.
Yogurt with Live Cultures (If Lactose-Tolerant)
- Why it helps: Probiotics may support a calmer gut environment.
- How to use: Choose lactose-free or strained yogurt (often lower lactose). Start with ½ cup daily.
Papaya
- Why it helps: Contains papain enzymes that may aid protein digestion.
- How to use: 1 cup fresh papaya as a snack or dessert (watch portions if you’re sugar-sensitive).
Kiwi
- Why it helps: Natural enzymes and fiber type that can support regularity without heavy gas.
- How to use: 1–2 kiwis/day, great for morning routines.
Avocado
- Why it helps: Healthy fats, potassium, and generally gentle fiber—but watch portion (it’s moderate in FODMAPs in large amounts).
- How to use: ⅛–¼ avocado per serving for most people.
Cucumber
- Why it helps: Hydrating, low-FODMAP, soothing crunch.
- How to use: Add to salads, infuse in water, pair with yogurt dip (lactose-free if needed).
Berries (Strawberries, Blueberries, Raspberries)
- Why they help: Fiber that’s often better tolerated than dried fruit; antioxidants support gut lining.
- How to use: ½–1 cup with breakfast or a snack.
Quinoa
- Why it helps: Gluten-free whole grain alternative, usually low-FODMAP.
- How to use: Base for bowls instead of wheat pasta/kuskus; rinse well before cooking to reduce bitterness.
A Practical Debloating Plate
- Base: quinoa or white rice (if very sensitive)
- Protein: eggs, chicken, fish, extra-firm tofu (press well)
- Veg: cooked zucchini, carrots, spinach, or small-serve salad with cucumber
- Flavor: garlic-infused olive oil (low-FODMAP), ginger, lemon, herbs
- Sides: ½ cup lactose-free yogurt or a kiwi
- Drink: peppermint or fennel tea post-meal
Other Very Effective Bloating Remedies
Exercise (light and regular)
- 10–20 minutes of walking after meals moves gas forward and supports motility.
Limit Portions
- Smaller, more frequent meals beat large, heavy ones—especially for slow stomach emptying.
Eat and Chew Slowly
- Put the fork down between bites, chew thoroughly, and avoid talking while chewing to cut swallowed air.
Stay Upright After Eating
- Keep your torso at 90° or take a stroll for 15–20 minutes. Skip the couch-lie-down.
Abdominal Self-Massage
- Gentle clockwise circles for 5–10 minutes can help move gas along.
Treat Constipation
- Aim for daily soft stools: fluids, magnesium citrate/glycinate (if appropriate), kiwi/prunes (if tolerated), or discuss osmotic laxatives with your clinician.
Simethicone
- Can reduce surface tension of gas bubbles; useful for short-term relief in gas-dominant days.
What About Red Flags?
Bloating plus unintentional weight loss, persistent vomiting, blood in stool, fever, new nighttime symptoms, or age >50 with new-onset symptoms deserves prompt medical evaluation. Also check for celiac disease, lactose intolerance, SIBO, IBD, thyroid disorders, and medication effects when the pattern is severe or persistent.





